OVERVIEW
Purpose of the Mapping Component
This component of the education handbook will inform and educate readers on topics related to maps and mapping, including what a map is, why one is needed, an approach to mapping, mapping challenges, how to prepare currently used local service and procedure terms for mapping, modifiers, long descriptors and clinician descriptors, map maintenance, and the importance of documentation related to mapping.
Intended Audiences
This portion of the education handbook is relevant to all audiences, including
- Research organizations
- Local/national governments
- Local/national physician/doctor organizations/associations
- National information/standards and policy organizations
- Health information management professionals
- Others involved with the mapping process
- Physicians/doctors
- Analysts
Learning Objectives
After reviewing the content in the Mapping Component, the reader is expected to be able to:
- Explain what a map is and why it is needed.
- Describe the mapping process.
- Identify options for addressing mapping challenges.
- Explain the need for preparing (“cleaning”) source terms for mapping.
- Describe the role of modifiers and why they should be considered in the mapping process.
- Define two types of CPT® descriptors and their purpose.
- Describe map maintenance considerations.
- List what documentation should be kept about the mapping process and understand why documentation is important.
Modules
The Mapping Component includes seven modules and one appendix. The information in these modules will increase readers’ understanding about mapping from source terms to CPT descriptions and demonstrate the comprehensiveness and appropriateness of CPT content for physicians/doctors to capture quality service and procedure data. In addition, the appendix provides mapping resources.
Following is a brief description of the content in each module.
Module One: Introduction to Maps – Explains what a map is, why maps are necessary, and the need to identify map users.
Module Two: Mapping Process – Describes a “how to” approach to developing a map and additional information to support mapping.
Module Three: Cleaning Source Terms – Explains why currently used source terms need to be reviewed and how they may need to be edited prior to starting the mapping process.
Module Four: Modifiers – Explains how additional information, ie, modifiers, attached to a source term may need to be considered in the mapping process.
Module Five: CPT Descriptors – Defines Long Descriptors and Clinician Descriptors and how to select which descriptor type to use for mapping.
Module Six: Map Maintenance – Provides information on why it is important to keep maps current for the duration of their use and how the maintenance function is performed.
Module Seven: Map Documentation – Lists the various types of documentation required related to the mapping process and why the documentation is important.
Each module is structured as follows. Note that some sections may not apply to a specific module.
Introduction - An introduction to the topic being discussed and why it is important.
- Intended Audience – The intended audience for the module.
- Learning Objectives – A list of learning objectives that will be covered in the module.
Main Module Content – The main content may consist of five main sub-sections.
- Personnel – People who are involved in the topic.
- Tooling – Tooling and requirements that are required to apply the approach.
- Approach – The approach or methodology specific to a topic.
- Process – The interaction between personnel with other personnel and/or tooling.
- Challenges – Challenges associated with applying the approach.
- Practical Use Example – An example of how the approach has been used.
MODULE ONE: Introduction to Maps
Introduction
This module introduces readers to what a map is and why it is needed.
Intended Audiences
This module is relevant to all audiences, including
- Research organizations
- Local/national governments
- Local/national physician/doctor organizations/associations
- National information/standards and policy organizations
- Health information management professionals
- Others involved with the mapping process
- Physicians/doctors
- Analysts
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Describe what a map is.
- Identify the purpose of maps.
- Indicate why it is important to know who will use a map.
Introduction to Maps
Personnel
- Health information management professionals
- Others involved with the mapping process
- Physicians/doctors
- Analysts
Tooling
None applicable
Approach
Definition and purpose of maps
A map is the result of linking a source term set to a target term set. Maps can be developed for different uses. The use of a map should be consistent with the intended purpose of the target terminology. As well, the intended use of a map determines how local terms for which the same clinical meaning is not available in the target terminology will be handled. Therefore, the intended use for a map must be defined before the mapping process begins.
There are a number of different types of maps. One is where historical clinical data collected using a local term set (source) is mapped to clinical data to be collected using a new terminology (target).
The development of a map is an important piece of the work necessary to be completed when a new terminology, such as CPT® content, is adopted for use. In the case where a local term set exists, maps are used to:
- Identify descriptions in the CPT code set being mapped to (target) with the same or similar clinical meaning as terms in the local term set being mapped from (source).
- Provide a link between current data collected using a local term set and future data collected using CPT content.
- Retain the value of historical data by supporting data analyses over time.
- Support the development of physician specialty subsets.
- Support the development of new clinical reporting policies.
It is also important to identify who the intended users of the map are as different user groups will most likely require different information, documentation, and education about the developed map and how it is to be used. Different users may also have different involvement in the map development and maintenance process.
MODULE TWO: Mapping Process
Introduction
This module provides an overview of how mapping is completed in the situation where a local term set exists, and it is the source for map development.
Intended Audiences
This module is relevant to all audiences, including:
- Research organizations
- Local/national governments
- Local/national physician/doctor organizations/associations
- National information/standards and policy organizations
- Health information management professionals
- Others involved with the mapping process
- Physicians/doctors
- Analysts
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Describe the three main components of mapping.
- Explain the mapping process.
- Describe the user roles involved in mapping.
- Describe different types of matching.
- Define mapping correlation and cardinality.
- State the stages in the mapping process (mapping progress).
- Describe quality assurance checks.
- Explain why map traceability is important.
Mapping Process
Personnel
People who are involved in the mapping process are:
- Health information management professionals
- Physicians/doctors who act as resources to mappers
- Others who have been assigned mapping responsibilities
- Analysts
Tooling
Although mapping may be completed manually with the use of Excel spreadsheets, the activity is usually performed using a software mapping tool with automated and manual assistance and review functionality.
Advantages of a software mapping tool
The use of a software tool to assist in the mapping process supports:
- Automatically saving completed work.
- Making completed work accessible to other project team members for review and reference.
- Tracking all updates made to information collected for a source term.
- Facilitating the addition of notes specific to a source term for future reference.
- Facilitating flagging a source term for review by other project team members.
- Tracking complete vs incomplete mapping numbers.
- Enabling identification of specific specialty subsets in which mapped CPT® descriptions should be included.
- Providing easy reference to mapping completed for preceding source terms and following source terms being reviewed.
Approach
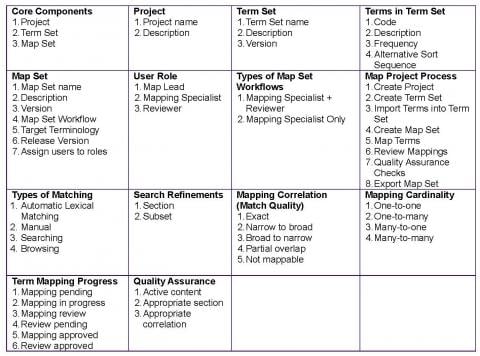
The following table provides an overview of each of the elements suggested to be included in the mapping process. They pertain to either manual or automated tool-assisted mapping. These elements are aligned to the approach based on SNOMED International mapping guidance, other key terminology organizations, and the literature. Detailed descriptions of each of these elements are provided in the following section.
Description of each mapping element
Core Components
Mapping consists of three main components:
- Project – A Project has a name and description. A Project can contain one or more Term Sets and Map Sets.
- Term Set – A Term Set is a collection of local terms that are to be mapped (source term). A Term Set has a name, description, and version. A Term Set belongs to a specific Project and contains a list of Terms (ie, code, description, frequency, and alternative sort sequence). A decision needs to be made on which terms will be included in the Term Set. As an example, perhaps terms related to payment are excluded from the Term Set or only terms that make up 90% of all terms used in the past five years are included in the Term Set.
- Map Set – A Map Set is the result of mapping a Term Set to a standardized clinical terminology (target term). A Map Set has a name, description, version, target terminology, release version, and language of target terminology, whether post-coordinated is allowed, and assignment of users to roles.
User Role
Personnel involved in the actual mapping process should possess defined skills and knowledge and be selected carefully. The mapping team should:
- Understand the content of the source terms and how they have historically been used.
- Understand the content of the target terms and their intended use.
- Be knowledgeable about the application rules for both source and target terms.
- Understand the use case for the map.
- Understand how the map will be implemented and who the users will be.
- Be confident in the use of any automated mapping tool to be used.
- Be able to identify any issues related to the creation and maintenance of the completed map.
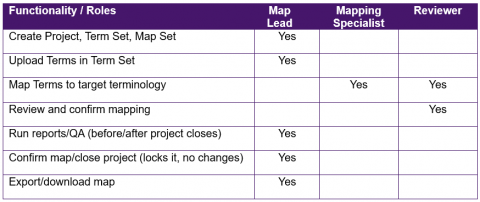
There are three main roles involved in the mapping process:
- Map Lead – Person(s) responsible for the overall map project.
- Mapping Specialist – Person(s) primarily responsible for mapping.
- Reviewer – Person(s) primarily responsible for reviewing and recommending changes to the mapping done by the Mapping Specialist. The Reviewer has final decision on the map.
In addition, a resource should be available to assist with clinical interpretation of either source or target terms during the mapping process to facilitate assigning the most appropriate target term possible.
A user can be assigned multiple roles. For example, the Map Lead can also be the Reviewer.
The following table describes the functionality available for each role.
Type of Map Set Workflows
There are two main workflows in the development of a Map Set:
- Mapping Specialist + Reviewer – Mapping is to be done by the Mapping Specialist and confirmed by a Reviewer. This workflow is the recommended workflow as a second individual is required to review each mapping.
- Mapping Specialist Only – Mapping is to be done and reviewed by the Mapping Specialist. It is recognized that some projects are very small with few individuals involved. In this case, a second individual is not required to confirm each mapping.
Overview Process
The following is a high-level overview of the mapping process from the creation of a Project until the map is exported. It is recommended that as a priority, the top 90% of service or procedure descriptions reported are mapped first with a decision then made about the need to proceed with mapping the remaining 10% of service or procedures descriptions reported.
- Create Map Project – A user creates a new Map Project with the goal of mapping a set or multiple sets of terms to various standardized clinical terminologies. For example, “General Surgery Mapping Project 2018.”
- Create Term Set – The user creates a new Term Set for the Map Project. The Term Set refers to the source terminology, which usually refers to local terms. For example, “Clinical Services.”
- Import Terms into Term Set – The local terms are imported into the Term Set via a tab-delimited text file, which can contain columns such as code and description. For example, “Code 1” and “Tonsillectomy.”
- Create Map Set – The user creates a new Map Set by identifying the Term Set to be mapped, the required workflow, the target terminology, release version and language (where applicable), and specifying users for each of the roles. For example, “Mapping Procedures to the CPT® Content.”
- Map Terms – Users assigned the role of Mapping Specialist proceed to map the terms in a Term Set.
- Review Mappings – Users assigned the role of Reviewer can proceed to review the mappings once Mapping Specialists specify via an indicator that a mapping is ready for review.
- Quality Assurance Checks – The Map Lead performs the final checks by running the built-in quality assurance checks.
- Export Map Set – The Map Lead closes the Map Set and exports the map in a tab-delimited text file or Excel file.
Types of Matching
Matching can be done automatically or manually. All automatic matching must be manually reviewed.
- Automatic – Automatic matching using lexical search algorithms.
- Manual
- Searching – Lexical searching.
- Browsing – Browsing target terms via a section structure.
Search Refinements
There are two main ways in which matching can be further refined or constrained:
- Section – Refining search results by the CPT code set sections.
- Subset – Refining search results to a specific subset.
Mapping Correlation (or Match Quality)
The mapping correlation allows a Mapping Specialist to indicate the match quality of the target term to a source term. Mapping correlation is important to know when data analyses are performed as it describes how well the source and target terms are aligned in clinical meaning.
There are five mapping correlations:
- Exact – The target term exactly represents the clinical meaning of the source term.
- Narrow to broad – The source term is more specific in its clinical meaning than the target term.
- Broad to narrow – The source term is less specific in its clinical meaning than the target term.
- Partial overlap – Part of the clinical meaning between the source and target term is the same but the source term contains additional meanings that are not found in the target term and vice versa.
- Not mappable – There is no target term available that is similar in clinical meaning to the source term.
Mapping Cardinality
Mapping cardinality may be computed automatically based on the number of target terms selected for a source term or assigned manually. Mapping cardinality is important to know when data analyses are performed to ensure that the correct source and target terms are included when longitudinal studies are completed.
- One-to-one – One source term is mapped to one target term.
- One-to-many – One source term is mapped to more than one target term.
- Many-to-one – More than one source term is mapped to one target term.
- Many-to-many – More than one source term is mapped to more than one target term (ie, the source term refers to multiple service or procedures descriptions resulting in mapping to multiple target terms).
Term Mapping Progress
- Mapping pending – Map Set task has been created but mapping of a term has not commenced.
- Mapping in progress – Mapping of a term has commenced by the Mapping Specialist but is not complete.
- Review pending – Mapping of a term has been completed by a Mapping Specialist and is pending review by a Reviewer.
- Mapping review – Reviewer has made comments or a change to a mapping, which is sent back to the Mapping Specialist for approval.
- Mapping approved – Mapping approved by Map Specialist.
- Review approved – Mapping approved by Reviewer.
Quality Assurance
The Map Lead can perform built in quality assurance checks once the mapping and review have been completed. This includes:
- Active content – Only active content in the target terminology is used.
- Appropriate section – A report on the top sections of the target terminology is generated to allow the Map Lead to determine if only the appropriate sections have been used.
- Appropriate correlation – Ensuring the appropriate correlation was used by comparing the target terms and correlation.
Traceability
It is important to be able to trace the evolution of a map from originally mapped target terms, any changes made to those terms, and agreement of final mapped terms. The evolution documentation should include personnel involved with mapping at various stages, the rationale for any changes, what the changes were, and final decisions. This traceability helps show the rigor involved with the mapping process and the thinking that went into determining the end map developed for actual use. This historical tracing of map evolution will help substantiate mapping decisions and may be a valuable resource should map target terms be questioned or challenged.
Challenges
The table below describes some of the challenges that may occur when performing the mapping process. Possible mitigation strategies are identified as well.

Not mappable source terms
Some source terms cannot be mapped to the CPT terms. Examples of common reasons why terms are not mappable are identified in the table below.
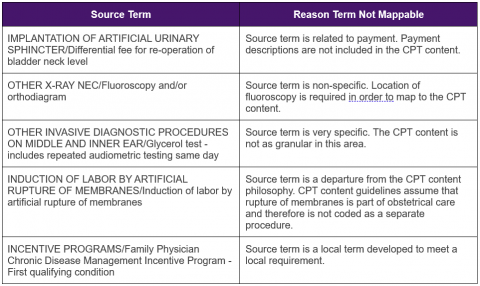
Source terms determined not to be mappable to the CPT content need to be identified as such for purposes of data analysis information. Guidelines should be established outlining how not mappable source terms will be handled. It is also useful information to know the frequency of reporting not mappable source terms and by which physician/doctor group(s) to help determine the magnitude of the issue and data impacted by the issue (eg, issue pertains only to orthopedic surgery).
MODULE THREE: Cleaning Source Terms
Introduction
This module describes the process followed to prepare source terms for mapping.
Intended Audiences
This module is relevant to all audiences, including
- Health information management professionals
- Physicians/doctors who understand the intent of source terms
- Others who have been assigned source term cleaning responsibilities
- Analysts
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Describe what cleaning is.
- Explain why cleaning source terms is important.
- Construct and apply cleaning rules.
Cleaning Source Terms
Personnel
People who are involved in the cleaning process are:
- Health information management professionals
- Physicians/doctors who understand the intent of source terms
- Others who have been assigned source term cleaning responsibilities
- Analysts
Tooling
Software tools may be programmed to identify inconsistent source terms that require cleaning and automatically apply cleaning updates based on predefined editorial guidelines. Manual review is required to ensure automated cleaning is done correctly and that all necessary updates have been made. All changes made to source terms need to be traceable.
Approach
Source terms may be developed for local use over multiple years by different authors. If detailed guidelines for term development are not documented or followed, inconsistency in term format and wording may easily result. These issues can make mapping to the CPT® content difficult.
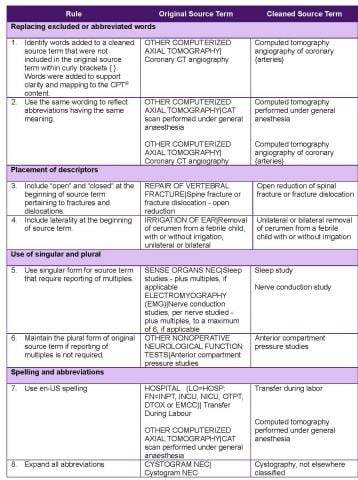
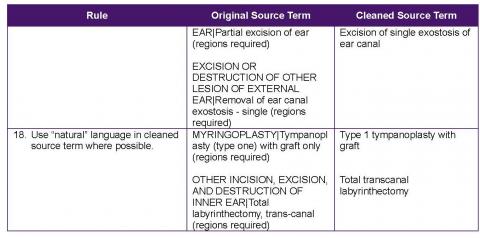
Before the mapping process begins, all source terms should be subjected to a review process with the intent to make sure common words (eg, open/closed) appear in the same position in a term, abbreviations are written in full, there is similar use of punctuation, etc. This process of review and standardizing the term descriptions is called “cleaning.” Established rules should be documented before the cleaning process begins. Each rule should be applied to a sample of source terms to validate their need, correctness, and applicability. Once the rules are agreed to, they should then be applied to the source terms. More rules may be required as the cleaning process is performed and additional issues are identified. These additional rules also need to be documented.
Challenges
Initially identifying which rules are required and getting agreement on their development and application by various stakeholders may be difficult. As a suggested approach, review the local terms first to understand what cleaning rules are required. Then draft a set of rules and develop examples of how applying the rules will facilitate mapping to target terms.
Practical Use Example
Some cleaning rules are identified in the table below. The rule is highlighted and followed by source term examples.

MODULE FOUR: Modifiers
Introduction
This module introduces readers to modifiers and their use.
Intended Audiences
This module is relevant to all audiences, including
- Health information management professionals
- Others who are involved with the mapping process
- Physicians/doctors
- Analysts
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Define what local and CPT® modifiers are.
- Understand the information that can be described with CPT modifiers.
- Identify options for handling local modifiers that need to be considered when mapping.
Modifiers
Personnel
People who are involved in assessing modifiers are:
- Health information management professionals
- Selected physicians/doctors who understand the intent of source terms
- Others who have been assigned source term cleaning responsibilities
- Analysts
Tooling
Data analyses are required to determine the historic use of modifiers, including frequency, trends (eg, use over time), who the users are (eg, restricted to one physician specialty), reason for use, etc. This work usually can be performed using a tool such as Excel.
Approach
Local modifiers
Sometimes, local modifiers may be used to further define a particular service or procedure or to identify the nature of the service. Modifiers may be clinical or non-clinical in nature with the resulting information used to support clinical data analyses or payment calculations. A decision needs to be made on how to handle local modifiers when moving forward with implementing the CPT content. This decision should be guided by detailed analysis of modifier data with subsequent discussion by stakeholders to confirm the need for modifier use. Modifier options to consider include the following:
- Analysis demonstrates that the information provided by the modifier is no longer required and modifier can be discontinued.
- Information can be derived from other reported data. For example, a modifier related to the age of a patient could be derived from a reported date of birth and date of service.
- Information, such as laterality, could be collected through a new data element.
- Information could be replaced with a CPT modifier.
- Because of the richness of CPT content, information is included as part of a CPT descriptor and a modifier is no longer required.
- Determine another means to capture non-clinical modifier information (eg, payment related) as only clinical information is reflected in the CPT descriptors.
CPT modifiers
A CPT modifier provides the means to report or indicate that a service or procedure that has been performed has been altered by some specific circumstance but not changed in its definition or code. The judicious application of modifiers obviates the necessity for separate procedure listings that may describe the modifying circumstance. Modifiers may be used to indicate to the recipient of a report that:
- A service or procedure had both a professional and technical component.
- A service or procedure was performed by more than one physician or other health care professional and/or in more than one location.
- A service or procedure was increased or reduced.
- Only part of a service was performed.
- An adjunctive service was performed.
- A bilateral procedure was performed.
- A service or procedure was provided more than once.
- Unusual events occurred.
Challenges
If not well documented, obtaining the history on the intended use of local modifiers may be difficult to obtain. How modifiers are interpreted and reported may vary from the intended use. The need to consider local modifiers in the mapping process may require analysis, discussions, and decision making by multiple stakeholders.
Practical Use Examples
Example 1
A physician providing diagnostic or therapeutic radiology services, ultrasound, or nuclear medicine services in a hospital would add modifier 26 to report the professional component.
73090 with modifier 26 = Professional component only for an X ray of the forearm
Example 2
Two surgeons may be required to manage a specific surgical problem. When two surgeons work together as primary surgeons performing distinct part(s) of a procedure, each surgeon should report his/her distinct operative work by adding modifier 62 to the same procedure code. For instance, a neurological surgeon and an otolaryngologist are working as co-surgeons in performing transphenoidal excision of a pituitary neoplasm.
Both surgeons would report:
61548 = Hypophysectomy or excision of pituitary tumor, transnasal or transseptal approach, nonstereotactic with modifier 62
MODULE FIVE: CPT Descriptors
Introduction
This module introduces readers to two types of CPT descriptors that should be considered when mapping local terms to the CPT content.
Intended Audiences
This module is relevant to all audiences, including
- Local/national governments
- Local/national physician/doctor organizations/associations
- National information/standards and policy organizations
- Health information management professionals
- Others involved with the mapping process
- Analysts
- Physicians/doctors
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Describe what CPT Long and Clinician Descriptors are.
- Explain the difference between the two types of descriptors.
- Evaluate the most appropriate descriptor type for mapping.
CPT Descriptors
Personnel
People who are involved in selecting which descriptors should be used for mapping are:
- Local/national governments
- Local/national physician/doctor organizations/associations
- Physicians/doctors
Tooling
A tool, such as Excel, is required to display Long Descriptors and related Clinician Descriptors for viewing and comparison. It is recommended a software mapping tool be used.
Approach
CPT long descriptors
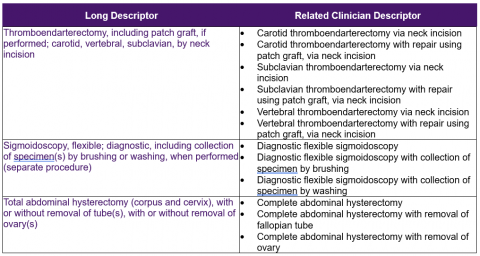
The CPT Long Descriptors refer to full descriptions of procedures as listed in the CPT Professional Edition book and approved by the CPT Editorial Panel. Although referring to one type of procedure, Long Descriptors may include more than one site (eg, nose and ears) or more than one mode of service (eg, needle and catheter). The Long Descriptor is not the most granular level of descriptor available in CPT content.
CPT clinician descriptors
CPT content includes a set of descriptors called Clinician Descriptors. According to the Clinician Descriptors README file:[1]
“The purpose of the Clinician Descriptors (CDs) is to clearly and specifically describe precisely the procedure or service performed by a physician or qualified healthcare professional at the point of care. CPT Clinician Descriptors will also reflect the granularity necessary to accurately describe clinically relevant information not included in the core CPT code set. As a result, many existing CPT codes will be mapped to more than one CD. These CDs will be easily understandable to the physicians or other qualified healthcare professionals who have little or no knowledge of coding and are primarily concerned with the clinical representation of the data rather than the administrative or reimbursement component of the data.”
There is often more than one Clinician Descriptor for each CPT code.
Long descriptors vs clinician descriptors
Mapping to either Long Descriptors or Clinician Descriptors should be determined by user need and stakeholder agreement. In most instances, as a starting point, source terms are mapped to Long Descriptors, especially if mapping is performed manually. Clinician Descriptors may then be determined from the mapped Long Descriptor. However, direct mapping to Clinician Descriptors may be performed with the support of a software mapping tool.
It may be beneficial to make both Long and Clinician Descriptors available in order to meet all stakeholders’ requirements. Those requiring information at a higher level may find Long Descriptors more useful while Clinicians may prefer access to Clinician Descriptors because of their granularity and their intent to be used at the point of care.
Challenges
Although Clinician Descriptors may be best suited for a particular use, because of their granularity, they may be more challenging to implement if there is no software system support available for data entry.
Practical Use Examples
Following are some examples of Long Descriptors and related Clinician Descriptors.
MODULE SIX: Map Maintenance
Introduction
This module provides information about why and how maps need to be maintained for the duration of their use.
Intended Audiences
This module is relevant to all audiences, including
- Local/national governments
- Local/national physician/doctor organizations/associations
- National information/standards and policy organizations
- Health information management professionals
- Physicians/doctors
- Analysts
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Explain why map maintenance is required.
- Describe what map maintenance includes.
- Explain what triggers an update to a map.
- Determine the point when a map is no longer needed.
Map Maintenance
Personnel
People who are involved in map maintenance and determining the date when a map will no longer be used are:
- Local/national governments
- Health information management professionals
- Selected individual physicians/doctors
- Analysts
Tooling
During the period that a map remains active, a tool such as Excel is required to identify additions, changes, or retirement of local terms or CPT® descriptors.
Approach
Changes are often made to the source term set and target term set to ensure they are up to date. This includes adding new terms to improve content coverage, inactivating terms that are no longer relevant, and changing terms to more accurately reflect service or procedures being represented. As such, there will be multiple data loads, mapping, and publishing cycles. Subsequent data loads require an additional step to ensure that any differences in either the map source or map target are accounted for with respect to existing maps, and any user reported errors or issues are addressed. To achieve this, a re-verification phase is necessary after a new map source or target is loaded. Changes in the map source or target should be determined, for example, description or term status changes should be identified, and if any changes affect existing maps then these maps should be marked as requiring re-mapping or reviewing. Changes to maps need to be documented and subject to audit. An audit of changes needs to be kept and circulated with or as part of the maps. On each release of the data, it is also important to ensure that there is an opportunity for the data owners to validate the results of the use of the maps when data stored in the originating terminology is migrated or transformed. Maps that are not properly maintained are likely to introduce errors.
In most cases, a designated time for sun-setting the map is necessary because it is no longer needed. This will always be important in the case of using a map to migrate one system to another. Once the migration has been accomplished, there is no longer a need to maintain the map. Any maps used for migration should be properly archived for reference if any questions arise concerning the migration project, use case, and business rules or associated heuristics.
Challenges
A process needs to be in place so those responsible for map maintenance are aware of changes made to local terms that may still be in use. As well, any updates to maps need to be distributed and implemented in systems. It may be difficult to monitor that updates have actually been implemented and that the correct map is applied to the data to which it pertains (eg, if a map is applicable to data for Year A, it should not be applied to data for Year B if changes have been made to the map for Year B).
MODULE SEVEN: Map Documentation
Introduction
This module provides reasons why documentation about mapping decisions and activities is important along with a list of topics that should be documented.
Intended Audiences
This module is relevant to all audiences, including
- Research organizations
- Local/national governments
- Local/national physician/doctor organizations/associations
- National information/standards and policy organizations
- Health information management professionals
- Physicians/doctors
- Analysts
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Explain why mapping documentation is important to complete and maintain.
- Understand the activities and decisions related to mapping that should be documented.
Map Documentation
Personnel
People who are involved in map documentation are:
- Local/national governments
- Health information management professionals
- Those involved with the mapping process
- Decision makers
Tooling
If available, a central repository where map-related documentation can be completed and stored is desirable. It is also desirable that the tool supports document traceability including authors’ names, versions, and dates of changes. Map stakeholders should have access to the documentation in the tool.
Approach
Keeping detailed documentation through all phases of mapping is critical. The documentation is a valuable resource as a historical reference and to substantiate decisions made. The documentation is also useful to demonstrate due diligence and support responses to any audit review.
Information that should be documented includes:
- Why the map was developed
- Intended purpose of the map
- Who should use the map
- Map tool selection process
- Source term set development process
- How source terms were prepared for mapping
- Who was involved with developing the map and reasons for their involvement
- The process followed to develop and quality assure the map
- Guidelines for accommodating not mappable source terms
- Rationale for mapping to Long Descriptors and/or Clinician Descriptors
- Definitions of mapping correlation and cardinality categories
- How any local modifiers were handled and how CPT® modifiers will be used
- Mapping challenges and how they were addressed
- Mapping heuristics
- Mapping resolution approach
- Map evolution traceability
- Map release notes
- Map roll-out plan
- Map maintenance process
Challenges
Documentation is often a neglected or forgotten task with its value not understood. It is important to clearly articulate documentation expectations and requirements at the onset of the map development process and hold people accountable for its completion.
APPENDIX: Mapping Information Resources
American Medical Association. CPT® Editorial Panel. The CPT® code process. Accessed at https://www.ama-assn.org/about/cpt-editorial-panel/cpt-code-process
Giannangelo K, ed. Healthcare Code Sets, Clinical Terminologies, and Classification Systems, 4th ed. Chicago: AHIMA; 2019.
Imel M, Giannangelo K, Levy B. Essentials for mapping from a clinical terminology. American Health Information Management Association (AHIMA), accessed at http://library.ahima.org/doc?oid=58226#.W9paWZNKjDd
International Health Standards Development Organization. Mapping to SNOMED CT: discussion and guidance on mapping based solutions design for migration or transformation. Accessed at https://confluence.ihtsdotools.org/display/DOC/Document+Library+File+List?preview=%2F73368648%2F73368662%2Fxdoc_MappingToSnomedCt_Current-en-US_INT_21030402.pdf