Overview
Purpose of the CPT® Primer Component
This component of the handbook informs and educates readers on the basics of CPT content, including its history and development, governance and maintenance, services and procedures covered, various types of descriptors included, uses, related support and products available, and benefits attainable from implementation.
Intended Audiences
This portion of the education handbook is relevant to all audiences, including
- Physicians/doctors
- Physician specialist groups
- Health service programs – quality improvement programs
- Health service delivery organizations
- Vendors of EMRs, EHRs, and specific clinical and functional areas
- Research organizations
- Local/national governments
- Local/national physician/doctor organizations/associations
- National information/standards and policy organizations
- Health information management professionals
- Those responsible for collecting service and procedure data
- Analysts
Learning Objectives
After reviewing the content in the CPT Primer Component, the reader is expected to be able to:
- Outline the history of CPT content development and ownership.
- Describe the CPT content maintenance process and release cycle.
- Describe the scope of services and procedures covered in the CPT content along with the purpose of Code Categories I, II, and III.
- Explain what Long, Clinician, and Consumer Friendly Descriptors are and state scenarios when their use is appropriate.
- Outline the various CPT resources available to support accurate service and procedure data collection.
- Understand the benefits possible with CPT® content use and describe the differences between CPT content and that of SNOMED CT®.
Modules
The CPT® Primer Component includes four modules. The information in these modules will introduce readers to essential material about CPT content and give them a foundation for moving forward with more detailed study in areas of interest to the reader.
Following is a brief description of the content in each module.
Module One: History, Governance, and Maintenance – Describes the development of the CPT content, how it is governed, and the rigorous process followed to add new content.
Module Two: Overview – At a high level, describes the services and procedures covered and the organization of the CPT Professional Edition book. The module also introduces the CPT content’s analytical and potential financial uses and ability to communicate uniform information about medical services and procedures among stakeholders.
Module Three: Resources – Informs the reader of AMA’s resources available to help accurately collect service and procedure data using CPT content. Also introduces the resource-based relative value scale (RBRVS), which is the physician payment system used by the Centers for Medicare & Medicaid Services (CMS) and most other payers in the United States. This system could be adapted for use outside the United States.
Module Four: CPT Content Benefits and Comparison to SNOMED CT® – Lists the uses and benefits of CPT content and provides a comparison of key attributes of CPT content to that of SNOMED CT®.
Each module is structured as follows. Note that some sections may not apply to a specific module.
Introduction – An introduction to the topic being discussed and why it is important.
- Intended Audience – The intended audience for the module.
- Learning Objectives – A list of learning objectives that will be covered in the module.
Main Module Content – The main content may consist of five main sub-sections.
- Personnel – People who are involved in the topic.
- Tooling – Tooling and requirements that are required to apply the approach.
- Approach – The approach or methodology specific to a topic.
- Process – The interaction between personnel with other personnel and/or tooling.
- Challenges – Challenges associated with applying the approach.
Practical Use Example – An example of how the approach has been used.
Module One: History, Governance, and Maintenance
Introduction
This module introduces the reader to the origin of the CPT content, its development and changing focus over the years. It also describes the governance responsibilities of the CPT Editorial Panel (the Panel), which ensures that CPT content remains up to date and the process is followed to introduce new service and procedure content.
Intended Audiences
As noted above in the Component Overview.
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Name the owner and maintainer of CPT content.
- Describe the evolution of CPT content.
- Describe the purpose and role of the CPT Editorial Panel as it relates to ongoing maintenance of CPT content.
- Explain the process followed to obtain approval for the addition of new CPT content.
History, Governance, and Maintenance
History
The CPT content is owned, maintained, and copyrighted by the American Medical Association (AMA). In 1966 the AMA published the first edition of what is now called the CPT Professional Edition book, which at that time focused on surgical procedures. The first edition sought to standardize terminology and reporting. The second edition, in 1970, expanded the scope. The third and fourth editions were released in the 1970s. The fourth edition was a major update and introduced a system for periodic monitoring and updating of the CPT content.
Governance
The CPT Editorial Panel is tasked with ensuring that CPT content remains up to date and reflects the latest medical care provided to patients. In order to do this, the Panel maintains an open process and convenes meetings three times per year to solicit the direct input of practicing physicians/doctors, medical device manufacturers, developers of the latest diagnostic tests, and advisors from more than 100 societies representing physicians and other qualified health care professionals.
The group has the final authority over all language within the CPT content.
Maintenance
The AMA-convened CPT Editorial Panel maintains the CPT content and consists of fifteen physicians and two qualified health care professionals (non-Doctor of Medicine and non-Doctor of Osteopathic Medicine). Currently only physicians from the United States are members of the CPT Editorial Panel. The CPT Editorial Panel also has minimum requirements on reviewing literature within US–based patient populations. The AMA Board of Trustees, responsible for implementing AMA policy, approves all nominations.
The CPT® Advisory Committee and the Health Care Professionals Advisory Committee (together the CPT/ HCPAC Advisory Committee or "CPT Advisors") support the CPT Editorial Panel. The CPT Advisory Committee consists of physicians nominated by national medical societies that are part of the AMA House of Delegates and HCPAC is composed of representatives of organizations representing qualified non-physician health care professionals. The AMA’s staff also provides an important role.
Although anyone may submit requests for updates to CPT content, it is often the physician specialty society or the organization representing qualified non-physician health care professionals that is most familiar with trends shaping a specific specialty who does so.
Proposals go through the following steps:
- Development of the initial proposal.
- The AMA staff reviews the proposal. This preparatory step confirms that the issue has not been previously addressed and that all of the documentation is in place.
- The CPT Advisors review the proposal. All are given the opportunity to comment, and those comments are then shared with all participants in the process, but not with the general public.
- The CPT Editorial Panel then reviews the code proposal at its regularly scheduled meeting. The group can accept as written, accept with modification, reject, table, or postpone the request.
- Approved Category I codes are then submitted to the Relative Value Scale Update Committee (RUC) for valuation.
All CPT Category III codes are subject to a process called "sunsetting." After five years, each Category III code is reviewed by the CPT Editorial Panel. If the original requestors of the code want to continue use of the code, they must submit a proposal for continuing the code as a Category III code or promoting it to Category I status.
Tooling
Not applicable.
Challenges
Although anyone may submit requests for updates to CPT content, currently only physicians from the United States are members of the CPT Editorial Panel. The CPT Editorial Panel also has minimum requirements on reviewing literature with US–based patient populations.
Module Two: Overview
Introduction
This module introduces the reader to the medical services and procedures described in CPT content and its key purpose of communication between stakeholders.
Intended Audiences
As noted above in the Component Overview.
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Describe the intent of CPT content and its three main components.
- Explain the breadth of medical services and procedures described in CPT content.
- Describe the intent of Code Categories I, II, and III.
- Name three types of descriptors and explain their purpose.
- Explain what Evaluation and Management (E/M) services are and in what circumstances they are used.
Overview
The CPT content is set of clinical terms including long, medium, short, clinician, and consumer friendly descriptors, codes, and thorough documentation and guidelines for their use. A robust set of educational resources is also part of the CPT content.
The CPT content describes medical, surgical, cognitive, and diagnostic services and is designed to communicate uniform clinical information about medical services and procedures among physicians/doctors, clinical staff, patients, accreditation organizations, and payers for administrative, financial, and analytical purposes.
Summary of CPT Content
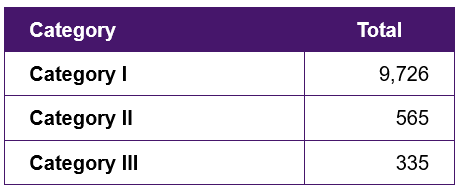
The following statistics provide an overview of the magnitude of CPT content and pertain to the CPT content release effective January 2021.
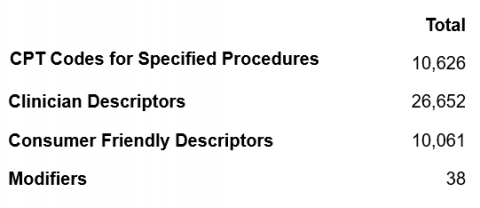
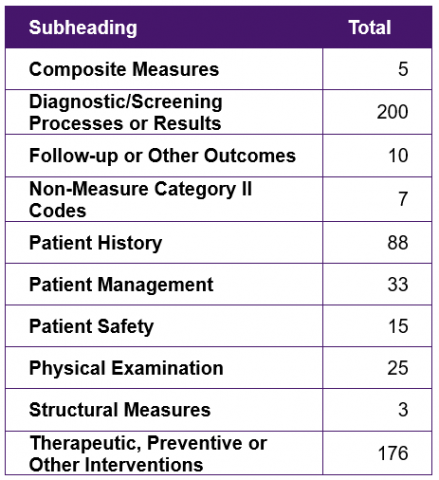
CPT CODES FOR SPECIFIED PROCEDURES BY CATEGORY
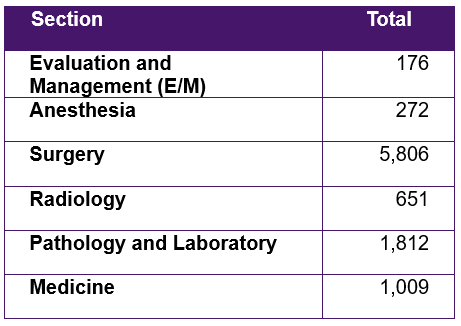
CPT CODES FOR SPECIFIED PROCEDURES BY SECTION
Category I
Category II
CPT Clinical Service Descriptors
First and foremost, CPT descriptors provide a uniform language that allows for accurately describing medical, surgical, and diagnostic services. CPT content covers the breadth of health services physicians/doctors provide. Descriptions for evaluation and management (E/M) services (such as a new patient office visit), anesthesia services, surgical procedures, radiology services, pathology and laboratory tests, and medicine are all found within the CPT® content.
The CPT content is divided into categories: Category I, Category II, and Category III. To be included in Category I or Category III, general and specific criteria must be met.
The general criteria that pertain to Category I and Category III codes are:
- The proposed descriptor is unique, well-defined, and describes a procedure or service that is clearly identified and distinguished from existing procedures and services already described elsewhere in the CPT content.
- The descriptor structure, guidelines, and instructions are consistent with current CPT Editorial Panel standards for maintenance of the CPT code set.
- The proposed descriptor for the procedure or service is neither a fragmentation of an existing procedure or service nor currently reportable as a complete service by one or more existing codes (with the exclusion of unlisted codes). However, procedures and services frequently performed together may require new or revised codes.
- The structure and content of the proposed code descriptor accurately reflect the procedure or service as typically performed. If always or frequently performed with one or more other procedures or services, the descriptor structure and content will reflect the typical combination or complete procedure or service.
- The descriptor for the procedure or service is not proposed as a means to report extraordinary circumstances related to the performance of a procedure or service already described in the CPT
code set. - The procedure or service satisfies the category-specific criteria set forth below.
Category I is the primary terminology included in the code set. It contains a description along with its five-character identifier for each service or procedure. Two-character modifiers are available to indicate the service or procedure performed has been altered by some circumstance but not changed in its definition. For example, the modifier 50 is used to indicate a bilateral procedure. CPT modifiers are relatively straightforward but are very important for coding accurately.
Specific criteria for inclusion in Category I include:
- All devices and drugs necessary for performance of the procedure of service have received US Federal Drug Administration (FDA) clearance or approval when such is required for performance of the procedure or service.
- The procedure or service is performed by many physicians or other qualified health care professionals across the United States.
- The procedure or service is performed with frequency consistent with the intended clinical use (ie, a service for a common condition should have high volume).
- The procedure or service is consistent with current medical practice.
- The clinical efficacy of the procedure or service is documented in literature that meets the requirements set forth in the CPT® code change application.[1]
Category I includes six main sections:
- Evaluation and Management (E/M)
- Anesthesia
- Surgery
- Radiology
- Pathology and Laboratory
- Medicine
The following example of a Category I service along with its identifier is found in the E/M section:
99244 Office consultation for a new or established patient, which requires these 3 key components:
- A comprehensive history;
- A comprehensive examination; and
- Medical decision making of moderate complexity
Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs.
Usually, the presenting problem(s) are of moderate to high severity. Typically, 60 minutes are spent face-to-face with the patient and/or family.
Category II CPT content is used for performance measurement. Category II CPT content was created to support data collection about the quality of care rendered by providers though the coding of certain services and test results that support US–established performance measures and that have an evidence base as contributing to quality patient care. They represent clinical findings or services where there is strong evidence of contribution to improved health outcomes and high-quality care. The use of these codes is optional. The codes are not required for correct coding and may not be used as a substitute for Category I codes.
Category II sections include:
- Patient Management: Describe utilization measures or measures of patient care provided for specific clinical purposes (eg, prenatal care, pre- and post-surgical care).
- Patient History: Describe measures for select aspects of patient history or review of systems.
- Physical Examination: Describe aspects of physical examination or clinical assessment.
- Diagnostic/Screening Processes or Results: Describe results of tests ordered (clinical laboratory tests, radiological or other procedural examinations, and conclusions of medical decision making).
- Therapeutic, Preventive, or Other Interventions: Describe pharmacologic, procedural, or behavioral therapies, including preventive services such as patient education and counseling.
- Follow-up or Other Outcomes: Describe review and communication of test results to patients, patient satisfaction or experience with care, patient functional status, and patient morbidity and mortality.
- Patient Safety: Describe patient safety practices.
- Structural Measures: Used to identify measures that address the setting or system of the delivered care. These codes also address aspects of the capabilities of the organization or health care professional providing the care.
- Nonmeasure Category II Codes: Codes are included for reporting of certain aspects of care. These factors are not represented by measures developed by existing measures organizations or recognized measures-development processes at the time they are placed in the CPT® code set but may ultimately be associated with measures approved by an appropriate quality improvement organization.
- Composite Measures: Combine several measures grouped within a single code descriptor to facilitate reporting for a clinical condition when all components are met. If only some of the components are met or if services are provided in addition to those included in the composite code, they may be reported individually using the corresponding CPT Category II codes for those services. An example of a composite measure code is:
- 0001F Heart failure assessed (includes assessment of all the following components):
- Blood pressure measured (2000F)
- Level of activity assessed (1003F)
- Clinical symptoms of volume overload (excess) assessed (1004F)
- Weight recorded (2001F)
- Clinical signs of volume overload (excess) assessed (2002F)
- 0001F Heart failure assessed (includes assessment of all the following components):
- Modifiers: Category II modifiers may be used for Category II codes to indicate that a service specified in the associated measure(s) was considered but, due to medical, patient, or system circumstance(s) documented in the medical record, the service was not provided. These modifiers serve as denominator exclusions from the performance measure. The user should note that not all listed measures provide for exclusions (see Alphabetical Clinical Topics Listing for more discussion regarding exclusion criteria).
The following is an example of a Category II code and descriptor:
4000F Tobacco use cessation intervention, counseling
Category III CPT content is for emerging technologies, services, and procedures. These codes may not conform to the usual requirements for CPT Category I codes, but allow physicians and qualified health care professionals, among others, to identify these technologies, services, procedures, and paradigms for clinical efficacy, utilization, and outcomes. They are considered "temporary," and they may or may not eventually be moved to Category I.
Every Category III code is reviewed by the CPT Editorial Panel five years from its publication in the CPT code set to ensure these temporary codes are still clinically relevant and necessary.
Specific criteria for inclusion in Category III include:
- The procedure or service is currently or recently performed in humans; and
- At least one of the following additional criteria has been met:
- The application is supported by at least one CPT advisor representing practitioners who would use this procedure or service; or
- The actual or potential clinical efficacy of the specific procedure or service is supported by peer reviewed literature, which is available in English for examination by the CPT® Editorial Panel; or
- There is (a) at least one Institutional Review Board-approved protocol of a study of the procedure or service being performed; (b) a description of a current and ongoing United States trial outlining the efficacy of the procedure or service; or (c) other evidence of evolving clinical utilization.
The following is an example of a Category III procedure that was subsequently converted to a Category I procedure. The Category III Sunset Date was January 2017.
0159T Computer-aided detection, including computer algorithm analysis of MRI image data for lesion detection/characterization, pharmacokinetic analysis, with further physician review for interpretation, breast MRI (List separately in addition to code for primary procedure)
The above procedure was deleted and converted to Category I status in January 2019 with the following two descriptions:
77048 Magnetic resonance imaging, breast, without and with contrast material(s), including computer-aided detection (CAD real-time lesion detection, characterization and pharmacokinetic analysis), when performed; unilateral
77049 Magnetic resonance imaging, breast, without and with contrast material(s), including computer-aided detection (CAD real-time lesion detection, characterization and pharmacokinetic analysis), when performed; bilateral
CPT Descriptor Types
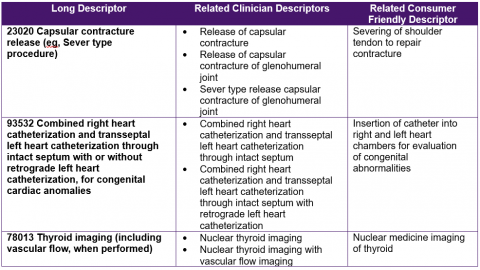
Long descriptors
A Long Descriptor is the full description of the CPT code as listed in the CPT Professional Edition book and approved by the CPT Editorial Panel. It is a technical description that fully describes the service or procedure provided. Although referring to one type of procedure, Long Descriptors may include more than one site (eg, nose and ears) or more than one mode of service (eg, needle and catheter). Analysts may find Long Descriptors useful when displaying information at a more summary level.
Clinician descriptors
A set of descriptors called Clinician Descriptors were designed to “describe clearly and specifically the procedure or service performed by a physician or qualified health care provider at the point of care."[2] They also may be used for "defining a subset of medical procedures and services within an electronic health record, patient summary for transition and transfer of care, documentation of medical procedures and services, research, clinical and statistical reporting etc."[3] There is often more than one Clinician Descriptor for each official CPT code descriptor.
Clinician Descriptors are clinician friendly terms that are usually more detailed descriptions of the procedure and reflect terms that physicians/doctors use on a daily basis.
Consumer friendly descriptors[4]
The goal of the Consumer Friendly Descriptors (CFDs) is to simplify the highly technical CPT Long Descriptors into something more patient focused and patient friendly. The AMA developed CPT CFDs, which take the complex terminology of medical procedures and services within the official CPT Long Descriptors and translates them into a language that a patient and/or caregiver can better understand and use. CFDs may prove useful in any situation where clear communication in non-technical language is important.
The responsibility of developing usable consumer content goes beyond constructing direct translations of the official CPT Long Descriptors. A consideration of the context of use is an important element in the development process. In the context of use for the patient, descriptive information that is relevant in the CPT Long Descriptor may not be relevant in the CFD. Rules and heuristics were developed to provide writers and reviewers guidance in development of CFDs with relevant information that considers the patient context.
EXAMPLES OF CPT DESCRIPTOR TYPES
CPT Content for E/M Services
Evaluation and Management (E/M) services encompass clinician services in a variety of locations and levels of service. Depending on the E/M service, certain factors must be known in order to select the best description to represent what service the physician provided. For example, patient/visit type may be a factor when deciding on the most appropriate health service description for the service rendered.
CPT content for E/M services is quite extensive. In fact, the CPT code set has a separate section, Evaluation and Management (E/M) Services, that contains the cognitive services commonly provided by physicians of any specialty.
Examples of services located in the E/M section include:
- Office or other outpatient visits
- Office or other outpatient consultations
- Inpatient consultations
- Hospital inpatient services
Multiple health service descriptions are available within the service categories. For example, there are three health service descriptions for inpatient subsequent care visits. Determining which of the three is the most appropriate to report is dependent on the patient’s status and the nature of the service provided.
The descriptors for E/M services provided recognize a number of components used in defining service levels. Key components used in determining levels are listed below.
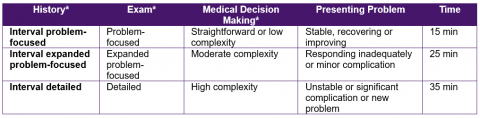
Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are considered contributory factors in the majority of encounters.
A significant change effective January 1, 2021, resulted in considerable streamlining of components used in selecting a service level of office or other outpatient visits, some of the most frequently used codes within this section. The changes will permit code selection based solely on medical decision making, or total time on the date of the encounter.
Within the E/M section are also health service descriptions for chronic care management services and transitional care management services. CPT content provides extensive information on what these services represent and how they should be reported. Following are excerpts from the CPT code set:[1]
Chronic care management services are provided when medical and/or psychosocial needs of the patient require establishing, implementing, revising, or monitoring the care plan. Patients who receive chronic care management services have two or more chronic continuous or episodic health conditions that are expected to last at least 12 months, or until the death of the patient, and that place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline. Code 99490 is reported when, during the calendar month, at least 20 minutes of clinical staff time is spent in care management activities. Code 99439 is reported in conjunction with 99490 for each additional 20 minutes of clinical staff time spent in care management activities during the calendar month up to a maximum of 60 minutes total time (ie, 99439 may only be reported twice per calendar month). Code 99491 is reported when 30 minutes of physician or other qualified health care professional personal time is spent in care management activities. Do not report 99439, 99490 in the same month as 99491. If reporting 99491, do not count any physician or other qualified health care professional time on the date of a face-to-face E/M encounter towards the time used in reporting 99491.
Complex chronic care management services are provided during a calendar month that includes criteria for chronic care management services including establishing, revising, implementing, or monitoring the care plan; medical, functional, and/or psychosocial problems requiring medical decision making of moderate or high complexity; and clinical staff care management services for at least 60 minutes, under the direction of a physician or other qualified health care professional. Medical decision making as defined in the Evaluation and Management (E/M) guidelines is determined by the problems addressed by the reporting individual during the month.
CPT® Guidelines
CPT guidelines are instructions, such as definitions, that provide clinical reporting information on a block of CPT content. Each section of CPT content has a set of guidelines as do many of the headings. For example, in the Medicine section, specific instructions are provided for handling unlisted services or procedures, special reports, and supplies and materials provided. Guidelines also provide explanations regarding terms that apply only to a particular section. For instance, Radiology Guidelines provide a definition of the unique term, "radiological supervision and interpretation," while in Anesthesia, a discussion of section-specific Physical Status Modifiers is included.
Following are some examples of CPT guidelines at the beginning of the Surgery section:[2]
- Follow-Up Care for Therapeutic Surgical Procedures: includes only that care which is usually a part of the surgical service. Complications, exacerbations, recurrence, or the presence of other diseases or injuries requiring additional services should be separately reported.
- Separate Procedure: Some of the procedures or services listed in the CPT Professional Edition book that are commonly carried out as an integral component of a total service or procedure have been identified by the inclusion of the term "separate procedure." The codes designated as "separate procedure" should not be reported in addition to the code for the total procedure or service of which it is considered an integral component.
However, when a procedure or service that is designated as a "separate procedure" is carried out independently or considered to be unrelated or distinct from other procedures/services provided at that time, it may be reported by itself, or in addition to other procedures/services by appending modifier 59 to the specific "separate procedure" code to indicate that the procedure is not considered to be a component of another procedure, but is a distinct, independent procedure. This may represent a different session, different procedure or surgery, different site or organ system, separate incision/excision, separate lesion, or separate injury (or area of injury in extensive injuries).
Parenthetical Notes
Parenthetical notes are instructions that verify the intent of the code(s). The notes are enclosed in parentheses within the CPT® content and may be found preceding or following a code listing and within a code descriptor. Instructions typically included as parenthetical notes with selected codes, indicate:
- Where to find a specific code
- When a code should not be reported with another code or codes
- When a code must be reported in conjunction with another code
These instructions are intended to prevent errors of significant probability and are not all inclusive.
For example, a code with such instructions may be a component of another code and therefore it would be incorrect to report both codes even when the component service is performed. These instructions are not intended as a listing of all possible code combinations that should not be reported, nor do they indicate all possible code combinations that are appropriately reported.
When reporting codes for services provided, it is important to ensure the accuracy and quality of coding through verification of the intent of the code by use of the related guidelines, parenthetical notes, and coding resources.
The following are some examples of CPT codes with parenthetical notes where not all procedures may be performed:
- 50545 Laparoscopy, surgical; radical nephrectomy (includes removal of Gerota's fascia and surrounding fatty tissue, removal of regional lymph nodes, and adrenalectomy)
- 52601 Transurethral electrosurgical resection of prostate, including control of postoperative bleeding, complete (vasectomy, meatotomy, cystourethroscopy, urethral calibration and/or dilation, and internal urethrotomy are included)
If the procedures in the parenthetical note were performed, do not report the codes separately. If not all of the procedures in the parenthetical note were performed, report the code and no reduction in service modifier is required.
CPT® License
The AMA holds the CPT copyright and use or reprinting of the CPT content in any product or publication requires a license. For AMA CPT Licensing information go to https://www.ama-assn.org/practice-management/cpt/ama-cpt-licensing-overview
Tooling
Although paper-based systems are able to accommodate CPT® content, implementation in an automated electronic medical record facilitates clinical term searches and ease of use across multiple stakeholders in the health care setting.
Challenges
Implementing CPT content would be an effort involving people and organizations across the health system. Challenges and risks are involved but those who have moved forward with implementation have not identified any insurmountable barriers to success. New implementers can build on lessons learned from others’ implementation of the CPT content.
Practical Use Examples
- The CPT content offers doctors a uniform process for coding medical services that streamlines reporting and increases accuracy and efficiency. For more than five decades, physicians/doctors and other health care professionals have relied on CPT content to communicate with colleagues, patients, hospitals, and insurers about the procedures they have performed.
- The descriptive terms and identifying codes within the CPT content currently serve a wide variety of important functions. This system of terminology is the most widely accepted medical nomenclature used to report medical procedures and services under public and private health insurance programs. The CPT content is also used for administrative management purposes such as claims processing and developing guidelines for medical care review.
- The uniform language is also applicable to medical education and research by providing a useful basis for local, regional, and national utilization comparisons.
- The CPT content captures quality and outcome measures — a feature that is likely to have increasing importance in the era of quality measurement.
- The CPT content is used to describe tests, surgeries, evaluations, and any other medical procedure performed by a health care provider on a patient.
- Like ICD codes, the CPT content is also used to track important health data and measure performance and efficiency. Government agencies can use the CPT content to track the prevalence and value of certain procedures, and hospitals may use the CPT content to evaluate the efficiency and abilities of individuals or divisions within their facility. As well, CPT content may be used to provide insights into trends, facility or provider performance, and population health.
Module Three: Resources
Introduction
This module provides information on a number of resources that are available through the AMA to assist CPT® content users with correct service and procedure reporting. For more information refer to Component 10, Educational Materials.
Intended Audiences
As noted above in the Component Overview.
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Understand the various CPT resources available through the AMA and be able to select the most suitable resource for an identified need.
- Explain the application of CPT® Link.
- Describe the Resource-Based Relative Value Scale (RBRVS)
CPT Resources
The AMA has a number of resources to help accurately report services and procedures. All AMA print resources are also available in eBook format. These are listed below.[3]
- CPT® Professional Edition: The CPT Professional Edition provides the AMA official guidelines to code medical services and procedures properly. Users can also request a CPT Data File license, which makes it easy to import codes and descriptions into electronic systems.
- CPT® Assistant: The monthly newsletter subscribers use to keep abreast of the latest codes, trends, and resources to help answer many coding-related questions.
- CPT® Network, including Knowledge Base, for Coding Inquiries: Quickly research the Knowledge Base (a database of commonly asked questions), view clinical examples (vignettes), and submit an electronic inquiry directly to CPT content experts.
- CPT® QuickRef: This mobile app helps physicians and qualified health care professionals select some of the most frequently used and arguably most difficult to assign codes: the evaluation and management (E/M) codes.
- Express Reference CPT® Coding Cards: Easy-to-use reference cards help health care providers and their staff quickly and easily find a CPT code. Twenty specialty cards are available.
- Principles of CPT® Coding: The full-color design of the illustrated ninth edition provides guidance on proper code application within each section of the CPT Professional Edition book. In addition, this reference contains chapters detailing the connection between and application of accurate coding, NCCI edits, and HIPAA regulations to documentation, payment, insurance, and fraud and abuse avoidance.
- CPT® Coding Essentials: Each of the ten titles within this series focuses on a subset of specialty-specific CPT codes and provides plain English descriptors, RVUs, modifiers, CCI edits, related HCPCS codes, ICD-10 crosswalks, and more.
- Medicare RBRVS: The Physicians' Guide: This reference provides the insights, tools, and tables needed to understand the Resource-Based Relative Value Scale (RBRVS) and how to assess the level of resources required for the majority of the procedures performed.
- Netter's Atlas of Surgical Anatomy for CPT Coding: Resource for surgical coding with integrated anatomical instructions and illustrations.
- Coding with Modifiers: Real-life modifiers scenarios and redacted medical records guide correct modifier usage so as to avoid costly payment delays and denials.
- CPT® Code/Relative Value Search: A free search (sign in required) for CPT codes and Relative Value Units. Users can perform up to five free searches per day.
CPT® Link
CPT® Link is a suite of CPT files containing explicit CPT hierarchies and CPT code properties as machine-processable readable attributes for use by software and application developers and advanced users. It is distributed through a variety of file formats:
- OWL (Web Ontology Language)
- XML (eXtensible Markup Language)
- Pipe-delimited text files
- Tab-delimited text files
- XSLX (Open XML spreadsheet) or more commonly referred to as Microsoft Excel files
CPT content is stored in four main files including Type, Property, Relationship Group (which includes the Relationship file), and Index. As an example, the Property file contains:
- Codes – Types of codes
- Descriptor – Types of CPT code descriptors
- Guidelines – CPT guidelines and parentheticals
- Flags – Attributes or properties about a CPT code
- History – Information about when an item first appeared and was last revised
- RVUs – Relative value units
- SNOMED CT – SNOMED CT concept identifiers and fully specified names
- Other – Other property types that do not fit in the previous categories
CPT® Link augments the standard CPT Data Files in a number of ways. For example, there are files that identify incremental and annual changes from the prior release. There are also files derived from the main CPT® Link data such as Coding Tips, Designations, and Guidelines. Additional files, for instance, include Edits and Index.
For more information refer to Component 8: CPT® Link.
Resource-Based Relative Value Scale
The Resource-Based Relative Value Scale (RBRVS) was developed during the 1986-1992 time period by a team of researchers at Harvard University. The goal of the system was to reflect what relative values would be under a hypothetical perfect market. The process of development was highly consultative and interactive throughout. Groups represented as participants in, or reviewers of, the work at various stages included AMA, physicians, government agencies, third-party payers, consumers, business, unions, and health services researchers. Numerous physicians played a key role, since the value of physician work was based on magnitudes estimated by doctors. Information from physicians/doctors was collected both through a large national random sample of practicing doctors and from smaller groups of expert physicians.
The value of a given medical service is measured in relative value units (RVUs) which have three components: physician work RVU, practice expense RVU, and professional liability insurance RVU. The sum of these three components, each adjusted for geographical cost differences, is the total RVU for a specific CPT® code. The total RVU is then multiplied by a dollar amount (called the Conversion Factor) to determine payment. The RBRVS is applied uniformly across all medical specialties and thus eliminates many disparities which arise when payments are specialty and practice specific.
The work RVU reflects the relative time and intensity associated with furnishing a service. In developing the RBRVS, estimates of the magnitude of physician work were made based upon typical cases, which were described within CPT content. Physician work is defined to include both time and intensity. Work time is divided into three time periods: pre-, intra-, and post service. Intraservice time for an invasive service is time spent actually performing a procedure; for other services, it is time face-to-face with the patient. Intensity includes three dimensions: mental effort and clinical judgment, technical skill and physical effort, and stress due to risk. Magnitudes were estimated by physician panels relative to a reference service in each specialty. Because each specialty used a different reference service, it was then necessary to put all specialties on the same scale. To do this pairs of services from different specialties, or “links,” which require the same amount of work, were identified and statistical techniques used to put different specialties on a common scale.
The practice expense (PE) RVU comprises the direct and indirect practice resources involved in furnishing medical services. This RVU accounts for the nonphysician clinical and nonclinical labor of the practice, as well as expenses for building space, equipment, and office supplies net of malpractice expenses. For many services two practice expense RVUs are provided. The non-facility setting practice expense refers to services performed in physician/doctor offices, freestanding imaging centers, or independent pathology labs. The facility setting practice expense is for all other settings, such as hospitals, ambulatory surgery centers, skilled nursing facilities, and partial hospitals. For services provided only in one setting, eg, a major surgery that must be done in the hospital only, the practice expense for that setting is provided.
The RVUs are periodically revised through a well-established process.
Tooling
EMRs, other automated tools for housing CPT content.
Challenges
Determining which resource(s) would best meet an identified need. Ensuring that once obtained, the resource is available to appropriate users and contents are interpreted and applied consistently.
Practical Use Examples
An individual responsible for collecting service and procedure data wants to know about CPT® content changes included in the latest release of the CPT code set. The CPT® Changes: An Insider’s View product provides this information.
A new version of the CPT content has been obtained and automated systems housing the previous version need to be updated to perform longitudinal analysis. CPT® Link contains the necessary data files.
Module Four: CPT Content Benefits and Comparison to SNOMED CT®
Introduction
This module provides information on the potential benefits resulting from CPT code set implementation and how the CPT content and SNOMED CT compare at a high level.
Intended Audiences
As noted above in the Component Overview.
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- State the benefits resulting from CPT content implementation.
- Explain key differences between CPT content and that of SNOMED CT.
CPT Content Benefits and Comparison to SNOMED CT®
Benefits of CPT Content
Following is a list of benefits that may be realized from implementing the CPT content.
- The CPT content has a broad range of uses including primary and secondary use and supporting policy development. It can also be integrated into analytical methods.
- Primary Use: Able to be used by physicians/doctors at the point of care.
- Secondary Use: Reported data can support quality measurement, performance parameters, and the billing and physician reimbursement process.
- Includes Clinician Descriptors, which were designed for clinicians to use to report the services and procedures they provide.
- Able to reflect patient complexity and intensity of services provided.
- Able to support innovative clinical practices and technologies.
- Includes comprehensive clinical content that reflects current patient services that can be used by all physicians.
- Includes descriptions tailored to meet physician specialty reporting needs (eg, anesthesiology, psychiatry) although any description may be used by any service provider (provider neutral).
- Supports accurate data capture by providing detailed and clear guidelines for correct description selection.
- Supports evidence-based accurate and trusted terminology with formal governance and strict review criteria.
- Editorial process is physician-driven, open, accurate, and transparent.
- The CPT content has a well-established maintenance process that is recognized and respected by users. Annual releases are frequent enough to keep up with changes in health care delivery.
- Supporting technical documentation, products, and assistance are available to help with CPT® content implementation and maintenance.
- Supports more complete and reliable data for administrative, financial, and analytical purposes.
- Includes Category II Supplemental Tracking/Performance Measurement codes/descriptions that are used for clinical quality improvement.
- There are AMA Express Reference CPT Coding Cards that list the most frequently used CPT codes for certain physician specialties, which may be considered subsets.
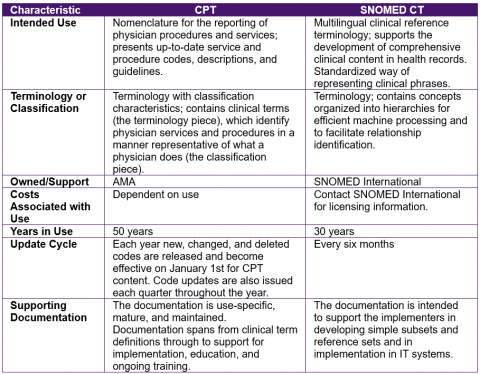
Comparison to SNOMED CT®
The CPT content is a set of clinical terms including long, medium, short, clinician, and consumer friendly descriptors, codes, and thorough documentation and guidelines for their use.
SNOMED CT® is an international clinical terminology; it is maintained and distributed by SNOMED International.
Key characteristics of the two terminologies are compared in the table below.
Tooling
Not applicable
Challenges
Implementing any new clinical content would be an effort involving people and organizations across the health system and presents challenges.
Practical Use Example
Example of CPT® content implementation includes the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP®).