Overview
Purpose of the RBRVS Component
This component of the CPT® Implementation Framework Education Handbook summarizes the relative value system, the role of the AMA/Specialty Society RVS Update Committee (RUC), the connection to Current Procedural Terminology (CPT®)[1] content, and describes uses of relativity measures.
Intended Audiences
This portion of the education handbook is relevant to all audiences, including
- Physicians/doctors
- Physician specialist groups
- Health service delivery organizations
- Vendors of EMRs, EHRs, and specific clinical and functional areas
- Research organizations
- Local/national governments
- Local/national physician/doctor associations/organizations
- National information/standards and policy organizations
Learning Objectives
After reviewing the content in the RBRVS Component, the reader is expected to be able to:
- Give a brief history of the RBRVS.
- Identify the RBRVS components.
- State the responsibility of the RUC.
- Summarize the RUC process.
- Generalize how CPT content is related to RBRVS.
- Provide illustrations of RVUs connected to CPT content.
- List an example of how RVUs may be used.
- Explain which RBRVS components are applicable for each use case.
Modules
The RBRVS Component includes four modules:
- Module One: RBRVS Background and Components – Summarizes the history and components of RBRVS.
- Module Two: RVS Update Committee (RUC) Role, Responsibility, and RVU Development and Revision Process – Explains the membership and responsibility of the RUC including the RUC process.
- Module Three: RVUs and CPT® Content – Describes the connection CPT content has to RVUs.
- Module Four: RVU Uses – Reviews how RVUs may be applied to determine physician workload and establish funding models. Practical use cases are described.
Each module is structured as follows. Note that some sections may not apply to a module.
- Introduction – An introduction to the topic being discussed and why it is important.
- Intended Audience – The intended audience for the module.
- Learning Objectives – A list of learning objectives that will be covered in the module.
- Main Module Content – The main content, which consists of five main sub-sections.
- Personnel – People who are involved in the topic.
- Tooling – Tooling and requirements that are required to apply the approach.
- Approach – The approach or methodology specific to a topic.
- Process – The interaction between personnel with other personnel and/or tooling.
- Challenges – Challenges associated with applying the approach.
- Practical Use Example – An example of how the approach has been used.
MODULE ONE: RBRVS Background and Components
Introduction
This module provides a summary of the history of RBRVS and describes its components.
Intended Audiences
As noted above in the RBRVS Component Overview.
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Give a brief history of the RBRVS.
- Identify the RBRVS components.
RBRVS Background and Components
The RBRVS was developed during the 1986-1992 time period by a team of researchers at Harvard University. Prior to that time, payment for each service was based on physician charges. The need for a new system grew out of the realization that the market for physicians was far from competitive and thus payments based on physician charges would result in distortions in payment rates between services. Consequently, the resource costs associated with physician work, practice expense, and professional liability insurance establish the RBRVS’s “relative value” of a given medical service.
Approach
The process of RBRVS development was highly consultative and interactive throughout. Groups represented as participants in, or reviewers of, the work at various stages included the American Medical Association (AMA), physicians, government agencies, third-party payers, consumers, business, unions, and health services researchers. Numerous physicians played a key role, since the value of physician work was based on magnitudes estimated by them. Information was collected both through a large national random sample of practicing physicians and from smaller groups of expert physicians.
The value of a given medical service is measured in relative value units (RVU) and has three components: physician work RVU, practice expense RVU, and professional liability insurance RVU. The sum of these three components, each adjusted for geographical cost differences, is the total RVU for a specific procedure, which is reported using a specific CPT® code. That is then multiplied by a dollar amount (called the Conversion Factor) to determine payment. The RBRVS is applied uniformly across all medical specialties and thus eliminates many disparities that arise when payments are specialty and practice specific.
The work RVU reflects the relative time and intensity associated with providing a service. In developing the RBRVS, estimates of the magnitude of physician work were made based upon typical cases, which were described within CPT® content. Physician work is defined to include both time and intensity. Work time is divided into three time periods: pre-, intra- and post service. Intra-service time for an invasive service is time spent actually performing a procedure; for other services, it is time face-to-face with the patient. Intensity includes three dimensions: mental effort and clinical judgment, technical skill and physical effort, and stress due to risk. Magnitudes were estimated by physician panels relative to a reference service in each specialty. Since each specialty used a different reference service it was then necessary to put all specialties on the same scale. To do this pairs of services from different specialties, “links,” which require the same amount of work, were identified and statistical techniques used to put different specialties on a common scale.
The practice expense (PE) RVU comprises the direct and indirect practice resources involved in providing medical services. This RVU accounts for the nonphysician clinical and nonclinical labor of the practice, as well as expenses for building space, equipment, and office supplies net of malpractice expenses. For many services two practice expense RVUs are provided. The non-facility setting practice expense refers to services performed in physician offices, freestanding imaging centers, or independent pathology labs. The facility setting practice expense is for all other settings, such as hospitals, ambulatory surgery centers, skilled nursing facilities, and partial hospitals. For services provided only in one setting, eg, a major surgery that must be done in the hospital only, the practice expense for that setting is provided.
The professional liability insurance RVU reflects the relative costs of professional liability insurance to practitioners. The Centers for Medicare & Medicaid Services (CMS) updates these RVUs annually based on a Medicare claims-based specialty mix for each service. CMS reviews the malpractice insurance premium data no less than every five years and adjusts the malpractice RVUs as necessary.
The RVUs are periodically revised by a well-established process.
MODULE TWO: RVS Update Committee (RUC) Role, Responsibility, and RVU Development and Revision Process
Introduction
This module describes what the RUC is, its responsibility, and the process the committee follows when developing or revising an RVU.
Intended Audiences
As noted above in the RBRVS Component Overview.
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- State the responsibility of the RUC.
- Summarize the RUC process.
RUC Role, Responsibility, and RVU Development and Revision Process
The AMA/Specialty Society Relative Value Scale Update Committee (RUC) plays a major role in the updates to physician work and direct practice expense valuation.
Approach
The RUC “provides medicine a voice in describing the resources required to provide physician services.”[2]
Of the RUC’s 31 members, 21 are appointed by a major medical society. An additional four seats, including one reserved for a primary care representative, two reserved for an internal medicine subspecialty, and the remaining seat for any other specialty society not a member of the RUC with the exception of internal medicine subspecialties or primary care representatives, rotate on a two-year basis. The remaining six seats include the chair and representatives of various organizations, such as the AMA, and committees, such as the Practice Expense Review Subcommittee.
Through a defined process, the RUC has the responsibility to make RVU update recommendations based on changes in medical practice to CMS for consideration.
RUC meetings are open to anyone who registers and signs a confidentiality agreement. The RUC meeting dates, locations, and minutes are posted on the AMA website.
The Advisory Committee to the RUC is comprised of one physician representative from each of the 124 specialty societies seated in the AMA House of Delegates. Members use a survey method developed by the RUC to present their societies’ relative value recommendations, which the RUC evaluates at the meetings.
Another group, the RUC Health Care Professionals Advisory Committee (HCPAC), provides the opportunity for limited license practitioners and allied health professionals (physician assistants, chiropractors, nurses, occupational therapists, optometrists, physical therapists, podiatrists, psychologists, audiologists, speech pathologists, social workers, and registered dieticians) to participate in the RUC process. A RUC HCPAC Review Board is responsible for developing relative value recommendations for procedures reported principally by non-MD/DO professionals.
A Practice Expense Subcommittee was established to assist the RUC by (1) addressing any practice expense policy issues and (2) reviewing practice expense inputs for new and revised codes and codes identified through the relativity assessment process or by CMS.
There is also a Relativity Assessment Workgroup responsible for identifying and assessing potentially mis-valued services as well as developing and maintaining all standards and procedures associated with the identification and reconsideration of the value of “new technology” services. Examples of mis-valued services reviewed include those with services that have experienced the fastest growth, services that have experienced substantial changes in practice expense, services where multiple codes are frequently reported in conjunction with furnishing a single service, and services where there may be a change in the typical site of service since it was last valued.
Other groups who support the RUC are the Administrative Subcommittee, Research Subcommittee, and Multi-Specialty Points of Comparison Workgroup.
The 2020 AMA RVS Update Process[3] booklet lists of series of steps used by the RUC for the revision process and summaries them in an associated diagram. They are provided below.
- Step 1: The CPT® Editorial Panel’s new or revised codes and CMS and RUC identified potentially mis-valued services are transmitted to the RUC staff, who then prepare a “Level of Interest” form. This form summarizes the panel’s coding actions and specific CMS requests.
- Step 2: Members of the RUC Advisory Committee and specialty society staff review the summary and indicate their societies’ level of interest in developing a relative value recommendation. The societies have several options: (1) they can survey their members to obtain data on the amount of work involved in a service and develop recommendations based on the survey results; (2) they can comment in writing on recommendations developed by other societies; (3) in the case of revised codes, they may decide that the coding change does not require action because it does not significantly alter the nature of the service; or (4) they may take no action because the codes are not used by physicians in their specialty.
- Step 3: AMA staff distributes survey instruments for the specialty societies. The societies are required to survey at least 30 practicing physicians. The RUC survey instrument asks physicians to use a list of 10 to 20 services as reference points that have been selected by the specialty RVS committee. Physicians receiving the survey are asked to evaluate the work involved in the new, revised, or potentially mis-valued code relative to the reference points. The survey data may be augmented by analysis of Medicare claims data and information from other studies of the procedure, such as the Harvard RBRVS study.
- Step 4: The specialty RVS committees conduct the surveys, review the results, and prepare their recommendations to the RUC. When two or more societies are involved in developing recommendations, the RUC encourages them to coordinate their survey procedures and develop a consensus recommendation. The written recommendations are disseminated to the RUC before the meeting and consist of physician work, time, and practice expense recommendations.
- Step 5: The specialty advisors present the recommendations at the RUC meeting. The Advisory Committee members’ presentations are followed by a thorough question-and-answer period during which the advisors must defend every aspect of their proposal(s).
- Step 6: The RUC may decide to adopt a specialty society’s recommendation, refer it back to the specialty society, or modify it before submitting it to CMS. Final recommendations to CMS must be adopted by a two-thirds majority of the RUC members. Recommendations that require additional evaluation by the RUC are referred to a Facilitation Committee.
- Step 7 The RUC’s recommendations are forwarded to CMS. CMS Medical Officers and Contractor Medical Directors review the RUC’s recommendations.
- Step 8: The Medicare Physician Payment Schedule, which includes CMS’s review of the RUC recommendations, proposals are published in July and finalized in November each year.
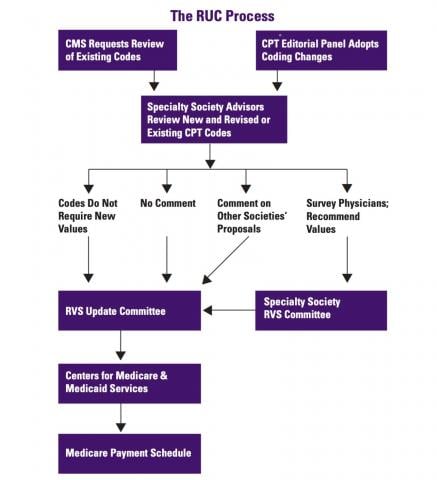
MODULE THREE: RVUs and CPT Content
Introduction
This module explains the connection CPT content has to RVUs along with several examples of RVUs for CPT codes.
Intended Audiences
As noted above in the RBRVS Component Overview.
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Generalize how CPT content is related to RVUs.
- Provide illustrations of RVUs connected to CPT content.
RVUs and CPT Content
The RBRVS is designed to work specifically with CPT content and includes a sophisticated physician work measure as well as a detailed measure of practice expense.
Approach
The relative values in the RBRVS were developed to correspond to the procedure definitions of CPT content. For new or modified CPT codes, a clinical vignette describing the typical patient and the service is created by the sponsoring medical society for the CPT code proposal application. Once approved by the CPT Editorial Panel, the code descriptor and clinical vignette are used by medical societies when conducting their surveys to determine the physician work and direct practice expense related to the CPT code. The survey also includes a reference list of CPT codes for specified procedures for comparison of time and estimation of work complexity/intensity to estimate the work RVU. For direct practice expense, survey participants are asked to identify a CPT code for a procedure that uses similar resources with regard to setting, clinical staff time, and medical equipment and supplies. There are several YouTube videos available on the RUC Survey Instrument.
- Understanding the RUC Survey Instrument – Physician Services without a Global Period (XXX-Global): https://www.youtube.com/watch?v=nu5unDX8VIs
- Understanding the RUC Survey Instrument – Surgical Services: https://www.youtube.com/watch?v=z1QFGVizeWs
- Understanding the RUC Survey Instrument – Non-Physician Qualified Healthcare Professionals: https://www.youtube.com/watch?v=kaw6-OhwbaM
The specialty advisors present the physician work and direct inputs for practice expense RVU recommendations and survey results to the RUC. After deliberations by the RUC, approved values are referred to CMS.
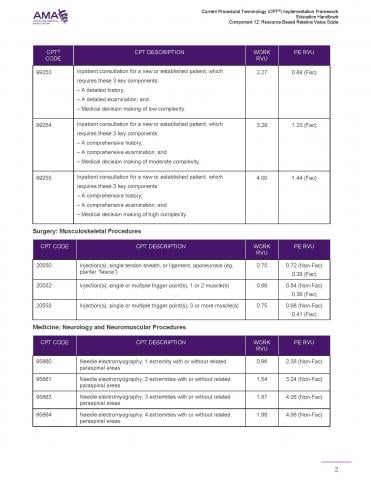
The following tables illustrate how the 2020 RVUs are connected to CPT content.

MODULE FOUR: RVU Uses
Introduction
This module reviews how RVUs may be applied to determine physician workload and establish funding models. Practical use cases are described.
Intended Audiences
As noted above in the RBRVS Component Overview.
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- List an example of how RVUs may be used.
- Explain which RBRVS components are applicable for each use case.
RVU Uses
The RBRVS has a number of uses. Two potential uses of an RVU are:
- Utilization of the RVU as a measurement of physician work
- Development of an RVU-based compensation or funding model
Approach
Measurement of physician work
The basic units of work for a physician procedure are much the same everywhere. Thus, the potential use of RVUs to measure physician work is possible by replacing the local term set with CPT® content. Simulation analysis can be conducted based on historical local/national claims data. The analysis relies on the terminology map which associates each current local health service description (including modifiers in many cases) with one or more CPT descriptions. Published data on relative value units gives the number of work RVUs and practice expense RVUs associated with a CPT code. Combining the local term set/CPT terminology map, the local/national claims data set, and the relative value scale data, it is possible to see for a specific type and amount of physician work what the current local/national units are for that work and also an estimate of what the work or practice expense RVUs would be for that same work if it were reported using CPT content.
Funding model
A physician fee schedule can be derived from the “relative value” of procedures provided and based on the resources they consume. For example, the US Medicare system and most other payers in the United States characterize physician work for purposes of fee-for-service (FFS) payment using CPT content. Payment amounts attached to each procedure are assigned using RVUs.
To reflect desired local/national payment policies, compensation under a local/national RVU-based model could be based on US RVU values adjusted by a group of factors deemed important for the jurisdiction.
A set of principles and goals for an RVU-based compensation system would include:
- Physician work should be a major factor in determining FFS compensation.
- FFS payments should cover overhead expenses.
- “Equal pay for equal work” is acknowledged as a guiding principle of payment equity.
- Methodology for determining compensation should be transparent.
- System should work well in the negotiated fee environment.
Core elements of the funding model involve:
- Physician work is to be measured by RBRVS work RVUs. The number of work RVUs from the RBRVS may be changed for use in the jurisdiction by payment adjusters.
- Overhead expense is to be measured by RBRVS practice expense RVUs. Types of facilities and the treatment of overhead in different settings may not be the same as in the United States, so it is recognized that facility and non-facility practice expense RVUs may need to be used in a modified form. For simulation work for example, use of non-facility practice expense RVU could be used for work done out of hospital and zero practice expense for work done in a hospital.
- The health effects and social impacts of particular services play no role in the RBRVS system. These aspects are, however, important in local/national thinking about what should determine physician compensation. While not affecting work units or practice expense, these could play a role in determining total RVU for a jurisdiction, using locally developed measures.
Some payments to physicians may not be closely related to the core elements, ie, physician work and overhead. Such payments, while important, are not specifically tied to individual health services and are not part of the RVU-based compensation system. Examples of such payments might include reimbursement of physicians’ travel expenses, incentives for providing services in remote or rural locations, or rewards for meeting specified performance or quality objectives. In the interest of transparency, supplemental payments should be described as to their intent and made apart from service fees rather than being included as payment adjusters. These are termed “supplemental payments” and noted as such as payment adjusters below.
One possible payment adjuster is modifiers. Some modifiers associated with a CPT® code for a specified procedure provide information about the service that could affect payment. Many of these modifiers are likely similar to current local/national modifiers. Second, some current local/national modifiers which now affect units and can be found are not analogous to modifiers in CPT content. Information represented by these modifiers could be used as payment adjusters, but this information would have to be provided in a way other than through CPT modifiers.
To determine if a CPT modifier would be useful for payment adjustment, a workgroup could be formed to review the full CPT modifier list and designate those which they thought would be most likely to be suitable for consideration as payment adjusters. Two members would complete this review and those modifiers which both respondents rated as likely would be considered in the initial workgroup discussion.
To guide the discussion, a common structure and type of information could be established. For example, if the US Medicare system specified a payment implication for a specific CPT modifier, it would be described, whether there was a local/national modifier similar to the CPT® modifier under consideration would be noted, and, if there was, whether a payment effect was specified in local/national documentation or suggested by analysis. The focus of the group then would be on the question: “Should this CPT modifier be used as a local/national payment adjuster?” If it was to be used as a payment adjuster, the type of adjustment should be discussed. Types of adjustment might be a change in the work RVU value, a change in the practice expense RVU value, a change in the dollars per RVU paid, or manual review and specific payment amount based on that review.
The following is an example of a group’s tentative conclusions regarding CPT modifier 22, increased procedural services, as a payment adjuster.
CPT Modifier 22 Increased Procedural Services
This modifier is to be submitted with documentation of additional work done. It was noted that this is similar to the Exceptional Circumstance health service code in the current local/national system. The tentative conclusion is that this modifier should be a payment adjuster and the type of adjustment would be manual review and specific payment decision based on that review reflecting an assessment of physician work involved.
Practical Use Examples
RVU Use – Physician Office Practice to Understand Clinical Workflow and Identify Potential Improvements
Dr. Merkel, a general practitioner in a physician group practice, is also responsible for some components of group practice management and clinical workflow across physicians in the office.
The questions he wants to answer are:
- How many patients were seen by physicians in the office each month over the last 3 months?
- How many services/procedures were provided to these patients during that time?
- What services were provided?
- What was the total work RVU for all services provided?
- What was the average work RVU per patient service?
- What was the total work RVU for services provided by each physician per month?
- What was the average work RVU for each physician?
- What was the difference across the physicians?
- Does this align with the desired clinical workflow?
- Where do changes need to be made?
In this case, the work RVU is the supporting measure used to represent physician work effort and is used with other clinical/provider information to support clinical workflow planning.
RVU Use – Surgical Group – Alternate Relationship Plans – Population Changes and Planning for the Future
The Baker Lake Orthopedic Physician Group (BL Group) has an alternate relationship plan/contractual agreement with the Ferry Central Health Authority (FCHA). As part of the agreement, BL Group is to provide orthopedic services to a range of patients across the local region and also provide inpatient orthopedic surgical services in FCHA.
Over the last 5 years, Ferry Central has become a popular retirement area and the demand for orthopedic services has changed. Recognizing this, FCHA has asked BL Group to work with them to project the future orthopedic service demand and what related orthopedic physician requirements would look like.
Working together, the questions FCHA and BL Group want to answer are:
- What was Ferry Central population over the last 10 years? How has this changed? What is the projected future population?
- What orthopedic services were provided to these individuals? How did this change over time? What would the future projection look like?
- What was the total, average, and service-specific work RVUs related to these services in the past? What would the future projections look like?
- How many orthopedic specialists were providing these services in the past and today?
- What are the expected patient, service volume, and work RVUs to be used as a baseline for what one orthopedic specialist can handle in a year?
- Based on the results of the calculations above, how many orthopedic specialists would be required each year for the next 5 years?
In this case, the work RVU is the supporting measure used to represent physician work effort and is used with other clinical/provider information to support health human resource planning.
RVU Use – Health System Policy Analyst – Cross Geographic Area Comparison to Inform Policy
A policy analyst with the national health system has been asked to do some policy analyses related to physician delivery of bariatric surgery across the country and the services delivered in the 3 months after surgery. All geographic areas currently use CPT® content as the standard for physician service clinical procedural reporting.
Questions the policy analyst wants to answer are:
- How many people have had bariatric surgery in the last year across the country, as identified by the physician clinical service reporting CPT codes 43770 – 43775, 43842-43850?
- How many physicians provided these bariatric surgery services? What were the total work RVUs related to these services?
- What physician services did these patients receive from the surgeon involved and other physicians in the 3 months after surgery?
- What were the work RVUs related to all physician services in the 3 months after surgery?
- For each geographic area:
- What was the distribution of the bariatric surgery patients, how many physicians provided the bariatric surgery service, and what were the total work RVUs?
- What was the average number of bariatric surgeries and related average work RVUs per physician?
- What was the total number of physician services and related work RVUs received from the surgeon and other physicians in the 3 months after surgery?
- For each person who had bariatric surgery, what was the average number of physician services and average physician service work RVUs in the 3 months after surgery?
- How do these results compare across geographic areas?
In this case, the work RVU is the supporting measure used to represent physician work effort and is used with other clinical/provider information to support understanding about physician clinical service need, delivery, and related work effort. This information could potentially inform clinical quality improvement.