Overview
Purpose of the Assessment of Feasibility Component
This component of the handbook educates readers on a methodology to use to complete an assessment of feasibility to determine, for the problems articulated in the project profile, if Current Procedural Terminology (CPT®)[1] content is the right solution.
Intended Audiences
This portion of the education handbook is relevant to all audiences, including
- Physicians/doctors
- Physician specialist groups
- Health service delivery organizations
- Vendors
- Local/national governments
- Local/national physician/doctor organizations/associations
- National information/standards and policy organizations
Learning Objectives
After reviewing the content in the Assessment of Feasibility Component, the reader is expected to be able to:
- State the initial starting point when assessing feasibility.
- Identify feasibility assessment questions.
- Give an example of a risk and mitigation strategy.
- Explain the four dimensions of feasibility.
- Identify criteria for each dimension.
- Describe a method to assess the dimensions.
- Identify the categories for determining if CPT content is suitable replacement for the clinical procedural content currently used for the uses selected.
- Explain what is included in each category’s criteria.
Modules
The Assessment of Feasibility Component includes three modules:
Module One: Overall Assessment Considerations – Describes the overall assessment considerations in determining feasibility.
Module Two: Dimensions of Feasibility – Defines the four dimensions of feasibility, the criteria for each dimension, and methods in which assessment may occur.
Module Three: Analysis and Evaluation – Explains a technique for gauging the suitability of CPT® content to meet the user’s need for clinical procedural content.
Examples of forms that could be used to conduct the feasibility assessment are included in the appendices.
Each module is structured as follows. Note that some sections may not apply to a module.
Introduction – An introduction to the topic being discussed and why it is important.
- Intended Audience – The intended audience for the module.
- Learning Objectives – A list of learning objectives that will be covered in the module.
Main Module Content – The main content, which consists of five main sub-sections.
- Personnel – People who are involved in the topic.
- Tooling – Tooling and requirements that are required to apply the approach.
- Approach – The approach or methodology specific to a topic.
- Process – The interaction between personnel with other personnel and/or tooling.
- Challenges – Challenges associated with applying the approach.
Practical Use Example – An example of how the approach has been used.
Linkages and Dependencies
The Assessment of Feasibility component has linkages and dependencies to the following:
- Framework: Provides an overview of the CPT® content uses.
- CPT Primer: Source for what is needed to understand CPT content, eg, what it is, what are the benefits of adopting CPT content, reasons for wanting to investigate CPT content, how CPT content compares to other terminologies and classifications.
- Licensing: AMA CPT Licensing overview information at https://cpt-international.ama-assn.org/importance-licensing-cptr-content
- Mapping: Describes a mapping approach for use in demonstrating the feasibility of mapping current content to CPT content.
MODULE ONE: Overall Assessment Considerations
Introduction
This module describes the overall assessment considerations in determining the feasibility to adopt and implement CPT® content.
Intended Audiences
As noted above in the Component Overview.
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- State the initial starting point when assessing feasibility.
- Identify feasibility assessment questions.
- Give an example of a risk and corresponding mitigation strategy.
Personnel
- Physicians/doctors
- Physician specialist groups
- Vendors
- Local/national governments
- Local/national physician/doctor organizations/associations
- National information/standards and policy organizations
- Analysts
Tooling
Interview guide to collect data on current state
Approach
Assessment of feasibility should start with a complete current state assessment of clinical procedural content collected, information flows, and processes, with the intent to better understand and document the starting points. This will involve assessment of current clinical procedural content, collection and storage processes, information flow mapping, and review and impact of any changes in clinical information. The interview guide is used to collect the data. The report serves a number of uses, such as a basis to understand potential impact on current clinical procedural data, eg, shifts between the actual services provided versus clinical procedural content being more accurately described.
In addition, the uses as they exist and future ones should be clearly articulated. Main categories are primary data use and secondary data use. The use case(s) serve as the backbone for the evaluation of CPT content to determine "fit for purpose." This will require gathering knowledge about CPT® content. Component 2, The CPT® Primer, provides this information. See the Framework Component for a description of use cases.
Process
There are three main questions to consider when assessing feasibility. They are:
1. Is the new clinical procedural content an improvement over the current clinical procedural content?
Improvement means two things: (a) The new clinical procedural content addresses, mitigates, or solves problems in the current clinical procedural content, which have been identified by stakeholders, and (b) the new clinical procedural content is more useful to specific user groups than the current clinical procedural content.
- (a) Identified problems: "Does the new clinical procedural content solve existing problems better than the current one?" An example of how this question could be answered is via a comparison of the way CPT content handles service intensity with the way the current terminology does it. Does CPT content better address the intensity?
- (b) Utility for specific groups: "Does the new clinical procedural content help the identified group do their job better than the current clinical procedural content?"
2. Does the investment in new clinical procedural content provide value? What benefits will be realized from the investment?
Value means the improvements derived from the new clinical procedural content are large enough to justify the expenditure it will cost to implement. Costs and benefits should be identified, and their magnitude estimated (in dollars or whatever measure that would be appropriate). In addition, the time at which they would be incurred will be estimated.
- (a) Costs typically would be incurred early in the implementation process. Examples include license royalty costs, the time and resources needed in implementing the new clinical procedural content, training people in its use, and all the supporting work needed to get it up and running.
- (b) Benefits typically are realized later once implementation is completed. An example of benefits includes reduced costs from identified problems. If the problems, eg, rejected claims or need for audits, are costly and the new clinical procedural content reduces the need for them, that cost saving is a benefit. Another possible benefit of the new clinical procedural content would be better quality data and increased use of the data. Expanded feedback to physicians resulting in their being able to do their work better is also a benefit.
3. What are the risks of proceeding and not proceeding with the use of new clinical procedural content for the stated use case(s)?
While the above questions evaluate expected improvements, costs, and benefits, risks are also associated with any large-scale project of this nature. Risks of not proceeding may include negative effects in the following areas: clinical service delivery, stakeholder relationships, clinical content, documentation, data-quality processes, and data/information use.
The following are examples of risks of proceeding and mitigation strategies that have potential significance to assessing feasibility and need to be considered along with improvements, costs, and benefits.
- Risk: The complexity and impact of the implementation are underestimated.
Mitigation Strategy: Continued identification and documentation of direct and indirect issues that arise during content development and implementation.
- Risk: Lack of CPT content experts.
Mitigation Strategy: Develop stakeholder expertise through development and delivery of targeted education and training programs, engage interested stakeholders in projects, needs assessments, focus groups, and working groups through all project stages.
- Risk: Loss of key staff.
Mitigation Strategy: Establish and develop a project team with adequate resources and knowledge to be able to withstand regular staff changes.
MODULE TWO: Dimensions of Feasibility
Introduction
This module defines the four dimensions of feasibility, the criteria for each dimension, and methods in which assessment may occur.
Intended Audiences
As noted above in the Component Overview.
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Explain the four dimensions of feasibility.
- Identify criteria for each dimension.
- Describe a method to assess the dimensions.
Personnel
- Physicians/doctors
- Physician specialist groups
- Local/national governments
- Local/national physician/doctor organizations/associations
- Analysts
Tooling
Analytical framework
Survey instrument to collect and analyze data
Approach
Once the current issues are fully understood and the uses documented, the appraisal is done. The three main questions described in Module One and summarized below should be considered during the critical appraisal.
- Is the new clinical procedural content an improvement over the current clinical procedural content?
- Does the investment in new clinical procedural content provide value? What benefits will be realized from the investment?
- What are the risks of proceeding and not proceeding with new clinical procedural content for the stated use case(s)?
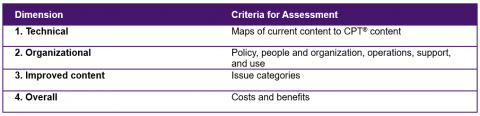
To proceed with these questions, a review of the four dimensions of feasibility—technical, organizational, improved content, and overall—would be beneficial.
Technical feasibility assessment is meant to answer the following:
Is replacement of the current clinical procedural content with CPT® content technically feasible? Would CPT content provide clinical descriptors useful for multiple purposes while enabling the linkage of data backward to preserve historical comparability for functions such as planning, monitoring, and auditing, which rely on longitudinal data use?
Organizational feasibility assessment is meant to answer the following:
Is replacement of the current clinical procedural content with CPT content organizationally feasible? Would it be compatible with the major principles of the health care system? Would the people and organizations that work with the content on a regular basis be able to adapt systems and processes to CPT content? Are there legal, institutional, or technological barriers to adoption of CPT content?
Improved content feasibility assessment is meant to answer the following:
Would CPT content represent an improvement over current clinical procedural content? Does it address identified shortcomings of the current clinical procedural content? Could it better describe the work physicians/doctors perform today and be more useful?
Overall feasibility assessment is meant to answer the following:
What would be the costs and benefits of making a change to CPT content? Is the return on investment with such a change viewed as favorable by stakeholders?
Process
Feasibility considerations may be assessed in the following ways:
1. Technical: A method for assessing technical feasibility is to determine the potential of CPT content to enable the linking of data backward to preserve historical comparability for functions such as planning, monitoring, and auditing. The procedural services from the clinical reference cases mentioned below, along with a group of procedural services frequently used by physicians/doctors, could be selected to determine backward compatibility. In addition, assessing technical feasibility may involve evaluating whether systems can accept the CPT code structure and subsequently the use of CPT content.
2. Organizational: A series of discussions with key stakeholders using an analytical framework may be used to evaluate this dimension. For example, the framework could consist of a number of system components grouped into categories:
- Policy (legislation and policy instruments),
- People and organizations,
- Operational processes (service delivery and claim submission to data analysis and use),
- Process supports (documentation, communication, education, and technology), and
- Uses of diagnoses and physician services data.
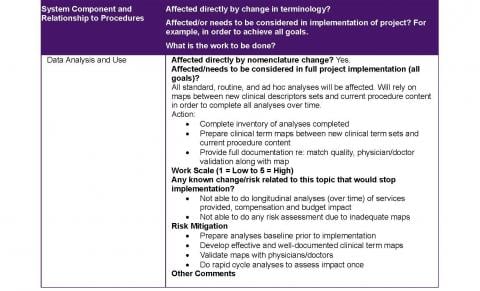
For each system component the assessment should consider whether or not the component would be directly affected by the adoption of CPT content, whether there would be any immediate or insurmountable barriers related to the component that would threaten implementation of CPT content, and how much work would be required as the project progresses through implementation and use of CPT® content. An example of assessing one of the system components is found in Appendix A.
3. Improved Content: To examine this dimension, specific comparisons between existing clinical content and CPT content based on reference cases is an option. The goal would be to provide stakeholders a basis for determining whether specific issues earlier identified as shortcomings of existing content are adequately addressed by CPT content.
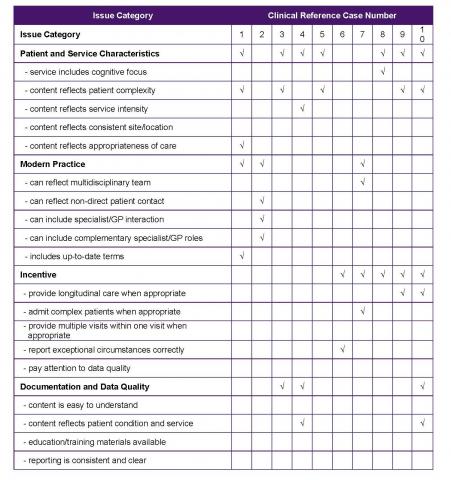
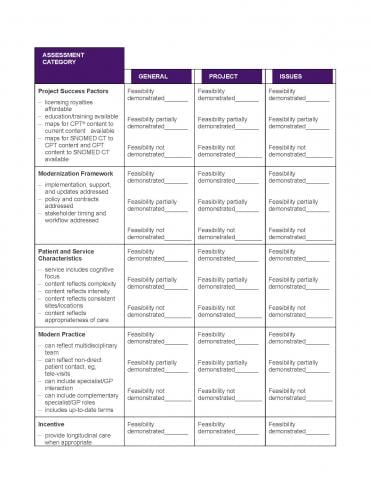
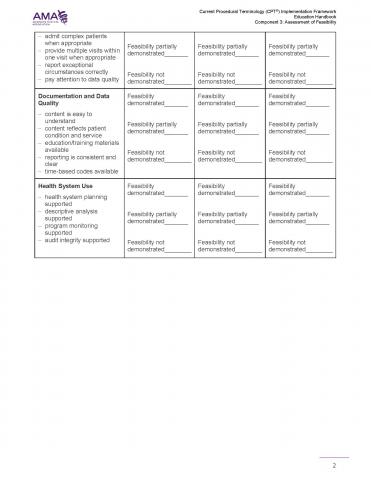
Criteria to develop clinical reference cases should be developed. To illustrate, one criterion might be to choose cases that illustrate issues identified by stakeholders in earlier interviews as problems with existing content or desirable features of new content. Issues may fall into categories such as patient and service characteristics, modern practice, incentives, documentation, and data quality. An example of an issue analysis grid is shown below:
4. Overall: There are a number of ways to evaluate costs and benefits of implementation.
When identifying benefits, one might conduct a benefits realization survey.
- Members could be asked to indicate (a) how confident they are that the benefit could be realized, (b) when they think the benefit would most likely start to be realized, and (c) how important they think the benefit is. An example is shown below:
- Benefit – Greater clinical effectiveness of health care delivery (eg, because doctors provided with better data about their patient populations are able to provide better care) | How much confidence do you have that this ultimate benefit will be realized?

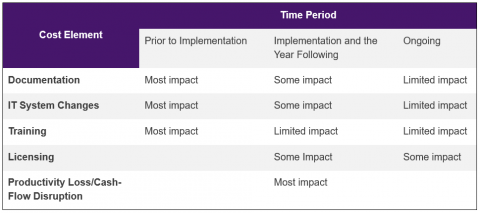
The major categories of costs will be training, documentation, IT system changes, licensing, short-term productivity loss, and possible cash-flow disruption.
- Discussions with the AMA about licensing requirements and associated royalties can help an organization better understand costs related to adoption of CPT® content. AMA CPT Licensing overview information is available at https://cpt-international.ama-assn.org/importance-licensing-cptr-content
The following summarizes the major cost elements and their timing:
Based on the above, criteria for each dimension are summarized in the table below:
MODULE THREE: Analysis and Evaluation
Introduction
This module explains a technique for gauging the suitability of CPT® content for clinical procedural content. A sample of a group evaluation form is found in Appendix B.
Intended Audiences
As noted above in the Component Overview.
Learning Objectives
After reviewing the content in this module, the reader is expected to be able to:
- Identify the categories for determining if CPT content is suitable replacement for the clinical procedural content currently used for the uses selected.
- Explain what is included in each category’s criteria.
Personnel
- Physicians/doctors
- Physician specialist groups
- Local/national governments
- Local/national physician/doctor organizations/associations
- Analysts
Tooling
None
Approach
With knowledge gained from the current state assessment, identification of CPT content use(s), and completion of the critical appraisal using the four dimensions described in Module 2, the next step in determining feasibility is to have the stakeholders use a specific set of criteria to collectively decide on the feasibility of adopting CPT content. This analysis and evaluation should focus on the following categories and criteria:
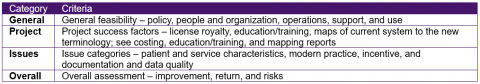
Based on the above criteria, one should be able to determine if CPT content is a suitable replacement for the clinical procedural content currently utilized for the uses selected.
Process
A technique for gauging the suitability of CPT® content for clinical procedural content is to perform a group consensus evaluation in which stakeholders collectively examine each issue category using materials prepared for each phase of the process. The group attempts to answer the question: "Has ability to address this issue category been demonstrated?" Appendix B shows how the results of the group process may be summarized.
APPENDIX A: Assessing Operations Processes
This appendix is an example of assessing the System Component: Operations Processes – service delivery, claim submission to data analyses, and use.
APPENDIX B: Feasibility Assessment Group Evaluation Summary Sheet
This appendix shows how the results of the group process may be summarized. A group consensus technique is where group members collectively examine each issue category using materials prepared for the process. The group attempts to answer the question: "Has ability to address this issue category been demonstrated?"
NAVIGATION
Component 3: Assessment of Feasibility
Component 7: Clinical Reporting
Component 9: Technical Requirements
Component 10: Educational Material